WithHealth: Launching a patient MedTech portal in six weeks
In just six weeks, we built a platform that ensured the safety of WithHealth's clients' workforce during the COVID-19 pandemic.
Learn MoreUltimate guide to custom healthcare software development in 2026
Last updated: December 16, 2025
Healthcare is undergoing a digital revolution, and artificial intelligence (AI) lies at its heart.
By 2025, AI-driven solutions are no longer experimental add-ons; they are becoming essential components of healthcare software. Hospitals and clinics worldwide are leveraging AI to streamline operations, enhance clinical decision-making, and improve patient outcomes.
A recent survey found that 86% of healthcare organizations already use AI in some capacity (HIMSS) , and over 73% of health executives plan to increase their AI investments (Fierce Healthcare).
The momentum is clear – for healthcare executives, understanding AI’s role in custom software is now mission-critical.
The healthcare industry is multifaceted. It comprises various subsets, each playing a crucial role in delivering comprehensive medical services. Let’s take a closer look at each of them.
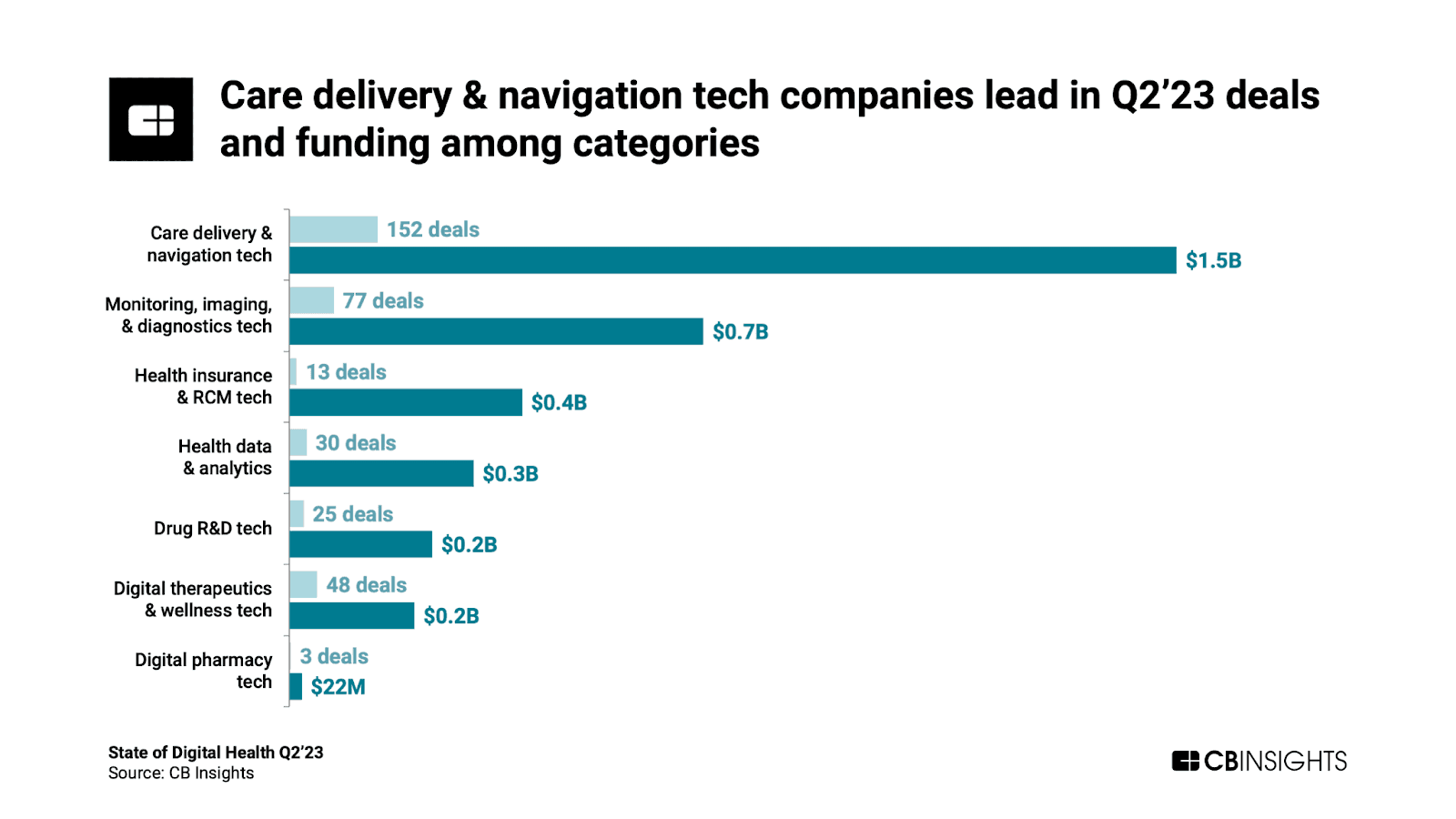
In the realm of healthcare, technology-driven solutions take the lead in enhancing the quality of care. Care delivery and navigation technologies aim to streamline healthcare processes, foster better communication between medical institutions and patients, and simplify the often intricate healthcare system.
The care delivery & tech sector puts emphasis on the use of tools such as electronic health records (EHRs), patient portals, telemedicine platforms, health information systems, patient engagement apps, and care coordination tools.
Within healthcare, another critical facet involves medical software solutions designed to monitor patient health, create diagnostic images, and identify diseases.
Here, remote patient monitoring systems, advanced medical imaging software, and laboratory information systems aid healthcare providers in delivering accurate and timely diagnoses.
Efficient healthcare delivery relies on the effective management of insurance claims and revenue cycles. Health insurance and revenue cycle management technology offer software solutions to health insurance companies and healthcare providers alike.
Examples of products within this subindustry include systems for processing health insurance claims and revenue cycle management software, ensuring the financial aspects of healthcare run smoothly.
In today’s data-driven world, healthcare organizations must harness the power of data to improve patient care and operations. The medical data and analytics subindustry steps in, providing software solutions that enable healthcare entities to collect, analyze, and visualize health data. These encompass health information exchanges (HIEs), clinical data warehouses, and population health management software.
Pharmaceutical innovation plays a pivotal role in healthcare advancement. This subindustry includes software solutions that help pharmaceutical companies develop and test new drugs through drug discovery software, clinical trial management software, and regulatory compliance software.
In the quest for holistic health, digital therapeutics and wellness technology take center stage. These software solutions are dedicated to treating and preventing diseases, as well as promoting overall health and well-being.
From mobile health apps to wearable devices and cognitive-behavioral therapy (CBT) software, these tools empower individuals to take charge of their health.
The subindustry of digital pharmacy technology offers software solutions designed to streamline pharmacy processes. These solutions include pharmacy dispensing systems and medication delivery apps, making the pharmacy experience more efficient and convenient for patients.
Market Segmentation: Healthcare software spans a broad range of solutions addressing different user groups and needs. It’s useful to view the landscape in three core categories – clinical, administrative, and consumer-facing software:
| Category | Purpose | Examples |
|---|---|---|
| Clinical Systems | Manage clinical information and workflows in patient care settings. Focus on improving diagnosis, treatment, and outcomes. | Electronic Health Records (EHR), electronic prescribing, clinical decision support systems, medical imaging software, telehealth consult platforms. |
| Administrative Systems | Streamline operational, financial, and back-office tasks for healthcare organizations. Aim to improve efficiency and reduce overhead. | Practice management software (scheduling, billing, claims processing), hospital information systems (HIS), revenue cycle management, supply chain management, staff rostering tools. |
| Consumer-Facing Applications | Engage patients directly and support self-care and patient-provider communication. Emphasize accessibility and experience. | Patient portal platforms, mobile health apps, wearable integration apps, remote patient monitoring dashboards, personal health record apps, wellness and fitness tracking apps. |
These segments often overlap – for instance, an integrated hospital platform may combine clinical and administrative functions, and many patient-facing apps tie into clinical systems. Nonetheless, this segmentation highlights the diverse use cases for custom software. Healthcare executives may target different segments based on strategic goals: improving clinical quality, achieving operational efficiency, or boosting patient engagement.
Healthcare executives are embracing AI-driven software, as clinicians increasingly work alongside intelligent systems to improve patient care and operational efficiency. AI innovations are transforming how healthcare is delivered and managed. Industry leaders anticipate significant returns: 71% of healthcare executives expect AI to boost profitability by 2025 (Exploding Topics). These expectations are grounded in measurable benefits.
For example, analysts estimate that wider AI adoption in U.S. healthcare could save $200–$360 billion annually through efficiency gains and prevention of costly events (Exploding Topics).
Such cost savings, combined with improved care quality, explain why the global AI in healthcare market is projected to soar to $164 billion by 2030 (up from ~$15 billion in 2024) (Markets And Markets).
Key drivers are converging to make AI indispensable: chronic staff shortages, rising costs, and ever-growing data loads. Frontline providers face burnout as administrative burdens mount – clinicians can spend up to 35% of their time on documentation alone.
At the same time, patients demand personalized, timely care, and payers emphasize value-based outcomes. AI-powered custom software offers a way to square this circle. It can automate routine tasks, surface insights from big data, and extend care beyond hospital walls. Notably, 92% of healthcare leaders believe automating repetitive tasks is crucial to addressing staff shortages (Exploding Topics).
In short, AI allows healthcare organizations to do more with less, without compromising quality or compliance.
For healthcare executives, the takeaway is clear: AI is no longer a “nice-to-have” – it’s a strategic imperative. Custom healthcare software development in 2025 is predominantly about integrating AI capabilities tailored to an organization’s unique needs. In the sections below, we explore the most impactful AI-driven innovations, the challenges to be mindful of, and best practices to ensure successful implementation. This guide will equip decision-makers with the insights needed to harness AI effectively in their healthcare software projects.
AI in healthcare spans a wide range of applications. Whether it’s automating back-office processes or aiding in clinical diagnoses, modern healthcare software increasingly embeds AI to work smarter.
Here we examine several AI-driven innovations that are reshaping healthcare software in 2025, and how they can be leveraged in custom development.
Healthcare organizations deal with countless repetitive, administrative tasks – scheduling appointments, processing insurance claims, managing billing cycles, and so on. AI “agents” and intelligent automation are revolutionizing these back-office operations. Rather than relying on human staff to handle every form or phone call, AI-powered software bots can take on much of the workload.
For example, intelligent automation systems (combining AI with robotic process automation) are now used to handle appointment scheduling, claims processing, and data entry with minimal human intervention (See” Intelligent Automation in healthcare: top uses cases in 2025). The impact on efficiency is striking: one hospital saw its AI-driven scheduling system cut patient no-show rates by 50.7% – ensuring patients get seen and revenue isn’t lost on empty slots (See: How AI reduces costs in healthcare organizations). In the billing department, AI can verify insurance eligibility and submit claims automatically, speeding up reimbursement. Oracle recently released a clinical AI agent aimed at automating healthcare administrative workflows, and NVIDIA launched customizable AI workflows for medical operations (NVIDIA)– signals that major tech players see huge opportunity in healthcare automation.
Case in point: Pragmatic Coders helped implement AI-driven features in WithHealth’s patient portal, saving the equivalent of one full-time employee’s workload – automating 40 hours of work per week (over 2,000 hours a year).
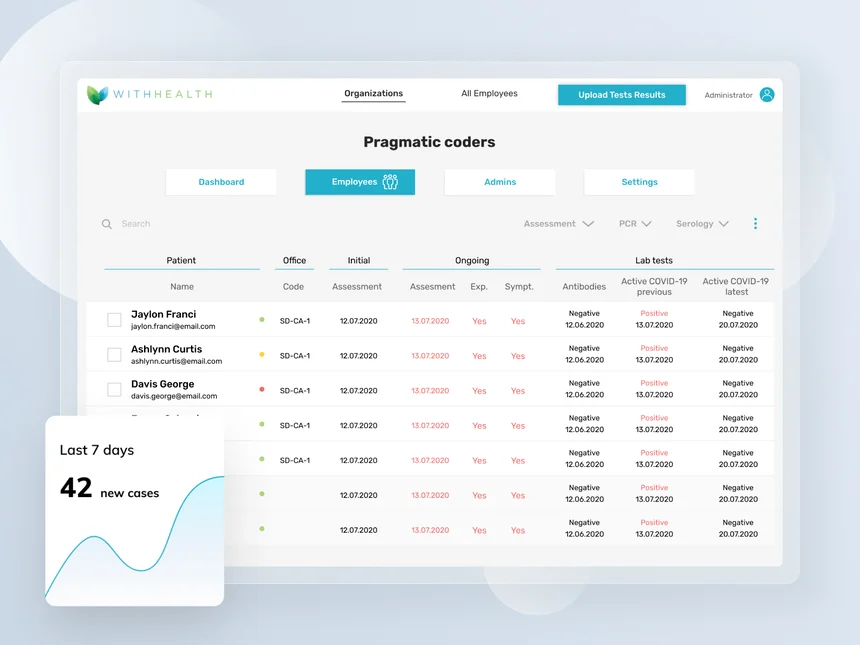
In just six weeks, we built a platform that ensured the safety of WithHealth's clients' workforce during the COVID-19 pandemic.
Learn MoreBy freeing staff from menial tasks, hospitals can reallocate manpower to more complex, value-added activities like patient care and research. Indeed, Gartner analysts predict that by 2025, the vast majority of providers will use AI in financial and administrative operations, leading to a 30% reduction in operational costs (Autonomix Solutions Inc).
The bottom-line for executives: custom software augmented with AI agents can dramatically improve throughput and accuracy in administrative processes, cutting costs and errors.
While operational automation yields quick wins, AI’s role in clinical decision support is equally game-changing. Modern healthcare software increasingly features AI algorithms that assist doctors in diagnosing diseases, interpreting medical images, and personalizing treatment plans. These tools do not replace clinicians, but rather augment their expertise with data-driven insights.
One prominent area is AI in medical imaging and diagnostics. AI models can analyze X-rays, MRIs, CT scans, and pathology slides far faster than humans – and often detect subtle patterns that the eye might miss. For example, AI tools for radiology can flag suspicious lesions or anomalies, helping radiologists prioritize urgent cases. Microsoft is working on new imaging AI models, and early implementations show that AI agents can dramatically speed up radiology workflows. In fact, observers are excited because AI could significantly shorten the turnaround time for MRI results, addressing a pain point in many healthcare systems. For example, in Poland, the waiting time for an MRI report has increased to 31 days, and for a CT scan to 22 days (Puls Medycyny).
Consistent with this, a recent study found that an AI-assisted digital stethoscope detected heart murmurs twice as effectively as traditional exams, enabling earlier diagnosis of valve problems (CBS News).
These examples highlight how AI-infused diagnostic software can improve accuracy and timeliness.
Another key innovation is the use of predictive analytics and machine learning on patient data. By analyzing electronic health records (EHRs), lab results, and even genomics, AI can identify risk factors and predict adverse events before they happen. Predictive algorithms enable a shift from reactive care to preventive care. For instance, if AI predicts a patient with chronic disease is at high risk of hospitalization, care managers can intervene early – preventing complications and costs. Healthcare providers are increasingly using such AI-powered risk stratification to manage populations with diabetes, heart failure, and other chronic conditions. In one case, AI-driven analysis helped an insurer (Oklahoma Health Care Authority) target interventions that led to a 24% drop in ER visits and 40% fewer hospital admissions annually per patient, saving over $1,500 per patient per year (Arine).
Custom software with these predictive features can give healthcare executives powerful tools to improve outcomes while reducing unnecessary utilization.
Ambient clinical intelligence deserves special mention as a new frontier in decision support. This refers to AI systems that listen and observe in the clinical environment to support clinicians. A prime example is AI that automatically transcribes and summarizes doctor-patient conversations in real time, generating clinical notes for the EHR. In outpatient clinics, such ambient AI assistants (often using advanced speech recognition and natural language processing) have been shown to cut documentation time from 2 hours to just 15 minutes in some cases (Nature).
One can imagine the impact on physician burnout and patient throughput when doctors spend less time typing and more time engaging patients. Tech solutions like Microsoft Dragon Copilot (prev. Nuance’s DAX Copilot), which listens to visits and drafts notes, are already being piloted in 2025. By integrating ambient intelligence into custom EHR software, healthcare organizations can dramatically reduce clerical burden while ensuring detailed, accurate records.
In summary, AI-driven decision support amplifies the capabilities of healthcare professionals. It helps catch problems early, make diagnoses more accurate, and keep clinicians focused on high-level decision-making rather than tedious analysis. Healthcare executives investing in custom clinical software should ensure that AI features – from diagnostic algorithms to smart charting assistants – are part of their roadmap. These enhancements translate directly into better patient outcomes and more efficient care delivery
One of the most exciting trends is the rise of ambient intelligence (AmI) in healthcare – essentially, smart environments embedded with sensors and AI that continuously monitor patient health in a background, unobtrusive way. This goes hand-in-hand with the growth of remote patient monitoring and Internet of Things (IoT) devices in medicine. Custom healthcare software in 2025 often extends beyond the clinic, integrating with wearables and ambient sensors to enable 24/7 patient monitoring and proactive care.

Medical dashboard for clinics | Pragmatic Coders
At Pragmatic Coders, we recently designed an AI-powered healthcare system for a network of clinics in the USA, enabling seamless patient service, medical record archiving, and real-time health data analysis. Through integrations with wearables like Galaxy Ring, Apple Watch, and portable blood pressure monitors, patient data is continuously gathered and analyzed remotely. This ensures that care teams have real-time insights into their patients’ well-being, helping them predict health risks and optimize treatment plans.
Ambient intelligence makes healthcare “surround” the patient much like ambient music – present everywhere but not intrusive. It leverages IoT sensors (wearable or in-room) plus AI analytics to track health signals in real time. For example, sensors in a senior’s home can detect if they fall or if daily activity patterns change. A company has developed a smart lamp called Nobi that does exactly this – it looks like a regular lamp but uses motion detection AI to sense falls and inactivity, automatically turning on lights and alerting caregivers if needed.
Another innovative solution, Kintsugi Voice, analyzes a patient’s speech for vocal biomarkers of depression or anxiety, enabling early mental health interventions. These ambient technologies feed continuous data to cloud-based healthcare software, where AI algorithms interpret the data and trigger alerts or recommendations.
Remote patient monitoring (RPM) platforms are also incorporating AI to enhance care between clinic visits. Wearables that track heart rate, blood pressure, glucose levels, oxygen saturation, etc., can generate a flood of data. AI is used to sift through this data and flag significant changes. This has proven benefits: remote monitoring of chronic conditions can prevent emergencies and save costs. In cardiac care, one program using AI-guided remote monitoring achieved cost savings of about €828 per patient per year by reducing hospitalizations (EP Europace).
In patients with COPD (a chronic lung disease), AI-assisted home monitoring led to a 44% decrease in emergency department visits by catching exacerbations early (Tenovi).
These outcomes are hard to ignore – they mean better patient health and lower expenditures on acute care.
Ambient and wearable AI technologies create a safety net around patients. They can alert clinicians to intervene before a minor issue becomes a crisis. Early detection and intervention are where huge savings and quality improvements lie. As one example, AI-enhanced telehealth systems now employ smart triage: patients’ symptoms are assessed by AI chatbots or apps before deciding if an in-person visit is needed. These systems have been shown to reduce unnecessary ER visits by up to 22% by directing patients to more appropriate care settings (PubMed Central).
Similarly, AI-powered telehealth platforms have cut appointment no-shows and improved access for rural populations, addressing care gaps while saving costs.
For healthcare executives, integrating ambient intelligence and RPM into your custom software means reimagining care delivery. Instead of episodic encounters, care becomes a continuous loop of monitoring, feedback, and intervention. Ambient AI systems in hospitals (sometimes called smart hospital solutions) can also improve safety and efficiency – think of environment-centric sensors monitoring room conditions, or computer vision that counts surgical instruments to prevent errors.
Even in the inpatient setting, ambient AI can track patient mobility or sleep patterns in the ICU to alert staff to subtle declines. The benefits of ambient AI include seamless patient experiences and early warnings for providers.
Custom health software can tie all these threads together, consolidating sensor data and AI insights into dashboards for care teams.
The bottom line is that AI extends the reach of healthcare beyond clinic walls. When building new healthcare solutions, consider how wearable sensors, voice assistants, and smart home devices might integrate with your software. The technology has matured to the point that ambient intelligence can offer reliable, clinically useful monitoring without burdening patients. This continuous care model not only improves outcomes but also aligns with reimbursement trends favoring preventive, holistic care. Executives who invest in AI-driven remote monitoring platforms today are positioning their organizations at the forefront of modern, proactive healthcare.
In 2025, patients expect healthcare experiences tailored to their individual needs – much like they experience personalization in retail or entertainment. AI plays a pivotal role in delivering personalized care at scale. Custom healthcare applications now often include AI-driven personalization engines, recommendation systems, and patient-facing chatbots that enhance engagement and adherence.
One aspect is precision medicine: AI can help customize treatment based on a patient’s genetic makeup, lifestyle, and past responses. For example, machine learning models can predict which medication or therapy is likely to work best for a particular patient, sparing them the trial-and-error. On a population level, AI can segment patients into subgroups to tailor interventions (for instance, identifying which diabetic patients would benefit most from a diet change vs. a medication change). Healthcare executives should consider how their software can incorporate such data-driven personalization features – whether through integrating third-party AI services or building custom algorithms on their own patient data.
Another aspect is AI-powered patient engagement tools. Think of the common scenarios: patients forgetting appointments, not adhering to medications, or feeling confused about post-discharge instructions. Here, AI chatbots and smart reminder systems can make a big difference. AI chatbots in patient portals can answer frequently asked questions 24/7, provide medication reminders, and even perform symptom checking to advise if a clinic visit is needed. This not only improves patient satisfaction (since they get instant responses) but also reduces the load on call centers.
We’ve seen these benefits firsthand in our work with an ethnic-aware patient management platform. One major challenge in the U.S. healthcare system is that providers often fail to account for cultural differences that impact care. For instance, in Somali communities, patients prefer doctors of the same gender, but many healthcare providers are unaware of this, leading to care gaps. Our AI-enhanced platform helped solve this by integrating demographic and psychographic data to improve patient engagement, compliance, and health outcomes. It also leveraged AI-powered predictive models to identify and address high-risk cases proactively. As a result, appointment no-show rates were significantly reduced (by roughly 30%), while personalized engagement improved patient adherence and satisfaction.
We built a patient management platform and an AI-powered data source for tailored care & deeper understanding of US minority communities.
Delivering a novel ethnic-aware patient care platform with AI & data science
Smart patient engagement systems driven by AI can also personalize content and outreach. For instance, an AI system might detect that a certain patient hasn’t logged their blood sugar readings recently and automatically send a nudge or alert to both the patient and their care manager. These systems create a more responsive experience, helping to keep patients on track. Crucially, better engagement translates to better outcomes – and cost savings. Missed appointments alone cost the U.S. healthcare system billions annually ($150 billion annually back in 2016, Healthcare Finance). As noted earlier, AI-based scheduling reminders cut no-show rates by roughly half (Science Direct), which for a large practice can recoup significant revenue. Furthermore, real-time language translation via AI (for hospitals serving diverse populations) can eliminate interpreter costs and improve communication, saving an estimated $279 per patient per year in interpreter expenses (PubMed Central) while making care more accessible.
From an executive perspective, custom software with AI-driven personalization is a competitive advantage. It can differentiate your patient services and improve loyalty. For example, consider a hospital that has an AI-enhanced mobile app: the app might proactively check in with chronic disease patients (“How are you feeling today? Do you need guidance on your diet or exercise?”) and then provide tailored advice or alert a nurse if needed. This kind of high-touch, personalized interaction at scale is only feasible with AI. Ambient intelligence plays a role here too – for instance, ambient sensors might adjust a hospital room’s lighting and temperature to a patient’s known preferences automatically, improving their comfort.
In summary, AI enables a shift from one-size-fits-all to one-size-fits-one in healthcare. Executives planning new software should ensure features like AI chatbots, recommendation algorithms, and personalized content delivery are on the feature list. Not only do these enhance patient experience, but they also drive better clinical compliance (e.g. medication adherence) and thus outcomes. The result is a virtuous cycle: engaged, satisfied patients who take charge of their health, leading to reduced readmissions and stronger financial performance for the provider
Fore more insights on the typology of medical apps, check 10 types of healthcare software in 2025 | Medical programs
Multiple forces in the healthcare industry are driving unprecedented demand for custom software solutions in 2025. Leaders should understand these macro trends to ensure their software initiatives align with broader strategic needs:
Value-Based Care and Outcomes Focus: Payment models are increasingly shifting from fee-for-service to value-based care, where providers are rewarded for quality and outcomes. This creates demand for software that can track quality metrics, integrate clinical and claims data, and support care management programs. Health plans report that nearly 45% of payments in 2023 were tied to value-based arrangements (Ahip), and this share continues to grow. Custom analytics tools, population health management systems, and care coordination platforms help organizations succeed under value-based contracts by identifying at-risk patients, closing care gaps, and reporting outcomes to payers.
Remote and Virtual Care Delivery: The pandemic-era boom in telehealth has transformed into a sustained push for remote care options. Patients expect convenient virtual access for routine consults, check-ups, and even chronic care management. Telemedicine usage remains far above pre-2020 levels, and providers are extending into remote patient monitoring (RPM) programs using connected devices. Medical software development is focusing on secure video visit platforms, at-home monitoring dashboards, and integration of IoT health data into clinical workflows. Telehealth and RPM are projected to be central pillars of care, with one analysis expecting 1.3 billion people to use digital health tools in 2024 (from fitness trackers to online consultations) (Statista). Custom solutions allow healthcare organizations to tailor virtual care to their patient populations and specialty needs.
Patient-Centric Engagement and Consumer Expectations: As patients take on the role of informed consumers, their expectations for service and convenience have risen. They want the “digital front door” experience – easy access to healthcare services through apps and websites, much like online banking or retail. 61% of healthcare consumers say that online appointment scheduling is extremely or very important when choosing a provider (Kyruss Health), and large majorities want digital options for tasks like paperwork, payments, and check-in. This trend drives demand for intuitive patient portals, self-service scheduling systems, mobile check-in and billing apps, and omnichannel communication tools (secure messaging, chatbots, etc.). Custom development enables organizations to design these tools in alignment with their brand and patient journey, integrating multiple touchpoints into a seamless experience.
Digital Health Investments and Innovation: Investors continue to pour capital into digital health startups and health IT innovations, even after the funding peak of 2021. Global digital health funding rebounded to $25.1 billion in 2024 (Galen Growth), indicating strong confidence in technology’s role in healthcare’s future. This influx of innovation is expanding what’s possible – from AI-driven diagnostics to novel digital therapeutics – and healthcare providers in turn demand custom software that can interface with or emulate these cutting-edge solutions. Moreover, big tech companies are actively developing healthcare platforms and APIs, raising the bar for interoperability and user experience. Health systems are partnering with or even acquiring tech startups to accelerate their digital transformation. In short, a culture of innovation has taken hold, and custom software projects are often the vehicles for bringing new ideas into practice, whether through in-house development or co-development with tech firms.
Workforce Challenges and Operational Efficiency: Healthcare faces chronic workforce shortages and burnout, particularly among clinical staff. Organizations are seeking technological solutions to automate routine tasks, reduce administrative burdens, and support clinicians. Nearly 49% of physicians report feeling burned out on a weekly basis (Chief Healthcare Executive), due in part to excessive documentation and clerical work – indeed, healthcare professionals spend up to 35% of their time on administrative tasks (PubMed Central). Custom software like intelligent scheduling systems, documentation automation, and workflow management tools can free up staff time. Additionally, analytics can optimize staffing and resource allocation. The drive to “do more with less” in a financially constrained environment makes efficiency-focused software a top priority for many executives.
These trends collectively explain why healthcare organizations in 2025 are heavily investing in custom software development. They need tailored solutions that legacy vendors or off-the-shelf products often cannot provide. Whether it’s to adapt to new payment models, engage digital-native patients, or relieve overstretched staff, custom software offers a path to address these strategic imperatives directly.
For more insights, check 19 must-know digital healthcare market trends for 2025
Healthcare leaders should view artificial intelligence as one vital tool in a larger toolbox of enabling technologies. In 2025, effective custom software solutions incorporate a blend of advanced tech capabilities and design principles. Below we explore several key technologies and enablers that are shaping healthcare software development.
In healthcare, the ability to share and integrate data across disparate systems is often the difference between fragmented care and coordinated, patient-centered care. Thus, interoperability is a cornerstone of custom software development in 2025. Healthcare executives are all too familiar with the pains of siloed data – for decades, electronic health records (EHRs), lab systems, pharmacy systems, and payer systems struggled to communicate. Today, that is changing rapidly thanks to standards and regulatory pushes:
For healthcare executives, investing in interoperability yields strategic benefits: it improves clinical decision-making (providers see a fuller picture of patient history), enhances patient experiences (not having to repeat the same information or tests), and even supports population health and research (larger unified datasets for analysis). Custom software should be built “interoperability-first,” adhering to standards and including capabilities to import/export data in common formats. The payoff is not just compliance with regulations, but creating a foundation that can plug into the wider digital health ecosystem instead of remaining an isolated tool.
In healthcare, software success is not judged by features alone but by adoption and usability. Clinicians and patients are notoriously quick to abandon clunky software. This makes User Experience (UX) design a critical enabler for custom healthcare software. A well-crafted UX can boost productivity, reduce errors, and delight users; a poor UX can render even powerful software unused. In 2025, there’s also growing emphasis on building a “digital front door” – an integrated online entry point that simplifies how patients access services. Key considerations include:
Clinician-Centric Design: For provider-facing systems, the goal is to streamline workflows and minimize clicks. Studies show that bad EHR UX contributes to physician burnout, whereas intuitive interfaces can save time. Custom development allows software to be tailored to how clinicians actually work, rather than forcing them into generic workflows. This might involve close user research and co-design with doctors and nurses. Features like voice recognition for hands-free charting (tied into ambient intelligence, discussed above), auto-filling of context when possible, and dashboard views that prioritize urgent info all contribute to better UX. For example, if designing a custom surgical checklist app, ensuring that it aligns with the surgical team’s real-world sequence and uses large, high-contrast buttons (for use in an operating room environment) can be the difference between enthusiastic uptake and frustration.
Patient-Friendly Interfaces: On the patient side, UX can determine engagement levels. A digital front door refers to a unified online experience where patients can accomplish a variety of tasks: find physicians, schedule appointments, complete registration forms, access telehealth, view results, and communicate – all through a common portal or app with a single login. The UX challenge is to make this experience as simple as using a consumer app. Efforts include providing self-service tools with clear prompts, offering choices in plain language (e.g., “I need a doctor” instead of jargon), and supporting multiple languages and accessibility needs. Given that many patients may have limited health literacy or tech literacy, UX designers aim to make interactions intuitive (e.g., using familiar icons and step-by-step guidance). In 2025, health systems report that digital front door initiatives are improving patient satisfaction and loyalty. One national survey found 50% of patients prefer engaging via a mobile platform for interacting with providers (Gozio Health), so meeting them where they are with excellent UX is crucial.
Omnichannel Engagement: Modern UX goes beyond just the app or website – it considers the entire journey. This includes how online and offline experiences connect. For instance, a patient might book an appointment online, receive an automated reminder text (with a link to directions), check in on a kiosk or phone upon arrival, and later get an email follow-up with lab results and a satisfaction survey. A seamless UX ensures each touchpoint feels connected (consistent branding, memory of user preferences, etc.). Custom software can be designed to support these omnichannel flows in a cohesive way, whereas siloed systems often lead to disjointed user experiences (like having to re-enter the same information at different stages).
Personalization: Executives are also recognizing the value of personalization in UX. Patients appreciate software that remembers their preferences – for example, a telehealth system that automatically offers an ASL interpreter if a patient is hearing-impaired and requested it before, or a portal that surfaces relevant preventive care reminders based on age/gender. Clinicians similarly value a dashboard that can be customized to their specialty or role (a cardiologist might want a different default view than a pediatrician). Custom-developed software can build in these personalization capabilities to drive higher engagement. (Learn more: 2025 guide to personalization in healthcare apps).
Investing in top-notch UX design and testing during development might increase project upfront costs, but it pays dividends in adoption and impact. For healthcare leaders, a key takeaway is that software is only as valuable as it is usable. This is especially true in healthcare, where users are often under high stress (ER nurses or anxious patients) – the software must be a help, not a hindrance. Making UX a first-class priority, possibly by involving UX researchers and designers early in the project, is now considered a best practice in healthcare software development.
Security and privacy are non-negotiable in healthcare software development. With sensitive personal health information (PHI) at stake and cyber threats on the rise, any custom solution must be built with rigorous safeguards from day one. Healthcare continues to be the industry with the highest data breach costs – the average healthcare breach cost reached $9.77 million in 2024 (The HIPAA Journal) – which can be devastating financially and reputationally. Key considerations for security and privacy include:
Compliance with Regulations (HIPAA, GDPR, etc.): In the U.S., the Health Insurance Portability and Accountability Act (HIPAA) sets strict rules for protecting PHI. Custom software handling patient data must implement the required administrative, physical, and technical safeguards – from user authentication and access controls to encryption of data at rest and in transit. In the EU and other regions, GDPR and local data protection laws impose additional requirements (e.g. handling patient consent, data residency). Regulatory compliance must be baked into the software design. For example, ensuring audit trails for data access (to know who viewed/edited a record and when) and features to support patient rights like data export or deletion when applicable. It’s wise to conduct privacy impact assessments during development and get legal/compliance teams involved early to avoid costly rework if the software is found non-compliant later. (Learn more: Essential guide to 2025’s HIPAA-compliant software development)
Robust Cybersecurity Measures: Healthcare organizations are prime targets for cyberattacks such as ransomware (as seen in multiple hospital shutdowns in recent years). Custom applications should follow best practices like secure coding standards, regular vulnerability scanning, and penetration testing. Using up-to-date encryption (e.g., TLS 1.3 for data in transit, strong AES encryption for databases) is essential. Multi-factor authentication (MFA) is increasingly mandatory for both clinician and patient access to systems, reducing risk if passwords are compromised. Additionally, principles of least privilege (users get the minimum access necessary) and segmentation (so a breach in one system doesn’t automatically open access to others) are critical in architecture. If the software integrates with devices or IoT, secure device management and data transmission protocols must be in place. Custom software often interfaces with older systems that might be less secure, so wrappers or gateways that add security layers to legacy integrations can be a good strategy.
Data Governance and Consent: Privacy is not just about breach prevention; it’s also about using data ethically and with consent. Custom software that aggregates patient data for analytics or AI should have governance rules encoded. For example, if using data for a research purpose, the software might need to de-identify it automatically or ensure only authorized researchers can access it. Patients increasingly demand transparency in how their data is used. Features like detailed privacy notices, consent management dashboards (where patients can opt in/out of data sharing programs) and fine-grained data access controls can differentiate a trustworthy platform. In 2025, with interoperability giving patients more control (via FHIR APIs and personal health apps), custom solutions should align with the philosophy that the patient owns their data. This means enabling easy and secure data sharing with patient-authorized third parties, but also protecting against any unauthorized access.
Incident Response and Resilience: Despite best efforts, breaches or outages can happen. Custom software should include audit logging and monitoring features that can help detect suspicious activity early (for instance, an unusual data access pattern). It should also be designed for resilience – e.g., backups, failover mechanisms, and contingency modes if a portion of the system must be shut down due to an incident. Having a built-in “read-only mode” if external connections fail, or a way to quickly revoke certain user privileges system-wide if a credential is suspected to be stolen, can be very valuable. Executives should ensure that any new custom system is integrated into the organization’s broader incident response plan and cybersecurity insurance coverage considerations.
Data security is one area where cutting corners can be disastrous. Aside from direct breach costs and fines, losing patient trust due to a privacy incident can irreparably harm an organization’s reputation. Conversely, a strong security posture can be a competitive advantage (patients and partners feel safer). In 2025, healthcare cyberattacks remain frequent, so assume any system will face attempted intrusions. Developers must stay updated on the latest threats and mitigation techniques (for example, protecting against ransomware that might try to encrypt cloud databases, or ensuring third-party libraries used in development are free of known vulnerabilities). Ultimately, security by design and privacy by design are mantras for custom healthcare software – every feature should be scrutinized through the lens of “does this expose data, and if so, how do we secure it?” and “are we handling patient information in a way that respects their privacy and meets legal requirements?”
To learn what types of digital health projects will get traction in 2025, check top 10 consumer healthcare startups to watch in 2025.
Effective healthcare is a team sport – it requires coordination across providers, specialties, and even across institutions. Likewise, improving health outcomes at scale involves managing the health of populations, not just individual episodes of care. Custom software in 2025 often aims to facilitate better care coordination and provide robust population health management (PHM) tools. These capabilities tie together many of the technologies discussed (interoperability, analytics, UX, etc.) to deliver the right information to the right people at the right time:
Integrated Care Coordination Platforms: Historically, it’s been challenging to coordinate patient care when multiple providers and settings are involved (for example, a patient transitions from hospital to rehab to primary care follow-up). Custom software can fill gaps by serving as a care coordination hub. Such a platform might consolidate a patient’s care plan, tasks, and communications in one place accessible to the care team (including external partners). Features often include secure messaging between providers (potentially replacing ad-hoc faxing and phone tag), shared care plans where each provider can update progress, and automated reminders for both patients and providers about follow-up actions. As value-based care grows, providers have incentives to ensure smooth transitions and avoid readmissions, making these tools very valuable. Modern coordination platforms also incorporate patient engagement – for instance, a discharge app that guides patients through post-op recovery steps and alerts a nurse navigator if the patient reports a concerning symptom. By 2025, many Accountable Care Organizations (ACOs) and integrated health systems have either adopted commercial care coordination software or built custom solutions to tailor to their network’s workflows and partnerships.
Population Health Analytics: On the population level, custom software is used to identify trends and manage cohorts of patients, which is critical for preventive care and chronic disease management programs. These population health tools ingest data from EHRs, claims, social determinants of health, etc., and provide analytics dashboards. Executives can see, for example, what percentage of their diabetic patients have their blood sugar under control or how many patients in a region skipped colorectal screenings. More advanced systems stratify risk (who is likely to incur high costs or have an adverse event) and even suggest interventions. The integration of AI is notable here – predictive models might, for instance, assess the risk of developing Alzheimer’s disease up to 10 years before symptoms appear (Alzai). Custom development in this arena allows organizations to include unique data sources or metrics that off-the-shelf products don’t support, and to embed the insights directly into clinician workflows (for example, showing a risk score in the EHR or triggering a case creation in a care management app).
Community and Social Care Integration: There’s increasing recognition that health outcomes are influenced by social factors (food, housing, transportation). Care coordination software is expanding to connect healthcare with community services. Custom solutions might include referral systems that allow a doctor or social worker to electronically refer a patient to a food pantry or transport service and track whether they received help – essentially extending the coordination beyond clinical care. Some health systems have built or adopted “social care platforms” and integrated them with their EHR. Custom development can ensure these platforms fit local community provider directories and capture relevant consent and data sharing agreements.
Collaboration and Data Sharing: Underlying good care coordination is data sharing, which ties back to interoperability. Custom software can create unified views (like a shared patient record across a region’s providers) even if the underlying systems are different, by aggregating the data. A trend in 2025 is also patient-mediated coordination – giving patients apps that aggregate their records and then allowing them to grant providers access.
An example is Health Folder, a digital solution we built to give patients control over their medical data, enabling them to securely store, access, and share records with healthcare professionals.
Such patient-centric approaches improve engagement and reduce administrative inefficiencies. Custom apps for specific conditions (e.g., oncology navigators) do this to ensure everyone sees the latest data (pathology reports, genetic tests, etc.). Secure cloud-based collaboration tools are also being used – for instance, tumor boards meeting via a virtual platform that shows all pertinent patient data and allows real-time input from multidisciplinary members. Developing such tailored collaboration tools can greatly speed up complex care decisions.
For healthcare executives, prioritizing care coordination and population health in software projects aligns with both quality imperatives and financial incentives. It directly supports reduced readmissions, higher preventive care uptake, and better patient satisfaction – key metrics in many contracts. It’s also part of building learning health systems, where the data from care is continuously analyzed to improve future care. The best custom solutions in this domain break down traditional silos between departments, providers, and even patients, creating a more transparent and connected care continuum.
Discover how Health Folder revolutionizes medical documentation management with its AI-powered mobile app built using low code.
Health Folder: Your AI-based digital medical documentation folder
Building a custom healthcare application is a significant undertaking that requires careful planning and execution to meet the unique demands of the healthcare environment. Below is a high-level overview of the process that healthcare organizations should follow to develop custom software successfully, from initial idea to launch and beyond:
Strategic Planning and Requirements Gathering: Begin with a clear understanding of the problem to solve or opportunity to seize. Engage stakeholders early – clinicians, administrators, IT staff, and patients (if applicable) – to gather requirements and pain points. Ensure the project aligns with the organization’s strategic goals (e.g., improving patient satisfaction or reducing costs in a specific service line). At this stage, define the scope and objectives of the software. For example, are you building a mobile app for chronic disease management or an internal workflow tool for referral management? Conduct market research to see if any existing solutions can be leveraged or if full custom development is warranted. Importantly, identify regulatory requirements upfront: determine if the software will handle PHI (almost always yes in healthcare) and thus need HIPAA compliance, or if it might be considered a medical device (requiring FDA oversight). This planning phase sets the foundation and should result in a detailed requirements specification and a business case/ROI analysis for leadership approval.
Design and Prototyping: Once requirements are clear, move into design. This involves system architecture design (choosing the tech stack, deciding on cloud/on-prem, database design, integration approach for existing systems) and UX/UI design. It’s highly recommended to create wireframes or prototypes of key interfaces – especially for user-facing components – and get feedback from end-users. For instance, before coding a patient portal, you might prototype the main screens (login, lab results, messaging interface) and have actual patients or staff review them. In healthcare, design should also account for accessibility (for patients with disabilities) and consider workflow design – mapping out how the software will be used in context (e.g., what does a nurse do first, second, third in using this tool during their shift?). Prototyping tools or even low-code platforms can be used here to simulate the application flow without full functionality, allowing iterative improvement of the design.
(Learn more: Why accessibility is important for your business)
Agile Development and Iteration: With designs in hand, development can begin. We use an Agile methodology – breaking development into sprints (typically 2 weeks each) and continuously delivering small increments of functionality. This approach is beneficial because it allows frequent check-ins with stakeholders and the flexibility to adapt to changes (which is common as users refine their understanding of needs). Early on, prioritize developing a Minimum Viable Product (MVP) – the smallest set of features that delivers value – so that it can be piloted. For example, if building a telehealth platform, the MVP might include patient login, video call, and basic documentation features, leaving more advanced scheduling or EHR integration for later sprints. Throughout development, maintain strong communication between the dev team and healthcare subject matter experts. Also, incorporate testing in each sprint (unit tests, code reviews, etc.) to ensure quality is built in gradually rather than slapped on at the end.
Testing, Validation, and Compliance Check: Healthcare software demands rigorous testing and validation given the high stakes. This goes beyond typical functional testing:
Deployment and Integration into Workflow: After thorough testing and necessary iterations, it’s time to deploy. In healthcare, deployment can be tricky because downtime can affect patient care. Often a phased rollout is wise: for example, introduce the software in one clinic or department as a pilot before scaling up organization-wide. This pilot acts as a real-world proving ground. Deployment tasks include setting up production infrastructure (ensuring all configurations are correct for security, connecting to live databases, etc.), migrating any needed data from old systems, and configuring user accounts and permissions. Equally important is change management – preparing the organization for the new software. This involves training sessions for users, creating user manuals or quick-reference guides, and having support staff on standby when the system goes live. Many projects use a “train-the-trainer” model where super-users (often clinicians who were involved in development or champions of the project) train their peers and act as first-line support. Integration into daily workflow also means possibly running the new system in parallel with old ones for a short period (to ensure nothing critical is lost) and then turning off legacy processes to fully transition.
Regulatory Compliance and Go-Live Checklist: Before officially going live, it’s prudent to do a final compliance review. Verify that all regulatory documentation is in place (for instance, update the organization’s HIPAA risk assessment to include this new system and its controls). Ensure that Business Associate Agreements (BAAs) are signed with any vendors or partners involved (like cloud providers or third-party service APIs used). Double-check that data backups are running and stored securely. Also, ensure any necessary patient or staff notifications are prepared if the new system changes how data is handled (for example, notifying patients of a new portal and how their information will be accessible). Once all is green-lit, execute the go-live. It’s often done during a low-volume period (overnight or weekend) for minimal disruption, with a clear fallback plan if something goes wrong (e.g., revert to the old system or have manual procedures temporarily).
Monitoring, Support, and Continuous Improvement: The development journey doesn’t end at launch. Post-go-live, set up continuous monitoring to catch any issues – this can include system uptime monitors, error logging alerts, and user feedback channels. Have a support plan: usually a helpdesk or on-call team for the first few days of launch when questions or bugs are most likely to surface. Gather user feedback systematically – perhaps through surveys or a built-in feedback tool – to identify enhancement opportunities. Then, iterate: plan regular updates or patches. In healthcare, you must also keep up with external changes; for example, if a new interoperability standard or billing code set comes out next year, the software should be updated accordingly. Many organizations schedule periodic improvements (monthly or quarterly releases) to continually refine the software based on analytics (like which features are underused and might need UI tweaks) and user input. Over time, measure the outcomes against the original goals – are we seeing shorter wait times, better patient engagement, cost savings, etc., due to the software? This will help demonstrate ROI and guide future development priorities. Essentially, treat the custom software as a product that needs ongoing care and governance.
By following a structured process like the above, healthcare leaders can mitigate the risks of custom development and greatly improve the chances of a successful outcome. Each step is important: skipping user input in planning or rushing testing, for instance, can lead to costly failures in a live clinical environment. Conversely, a well-executed development process produces software that truly fits the organization’s needs, is safe and effective, and has the buy-in of its users – all critical markers of success in healthcare.
Custom healthcare software development in 2025 is about seeing the big picture. While technologies like AI provide powerful new capabilities, true digital transformation comes from integrating multiple innovations – AI, cloud, interoperability, mobile, UX design, security, and more – into cohesive solutions tailored to the organization’s needs. Healthcare executives must take a strategic, balanced approach: leverage AI where it adds value, but also invest in the less-glamorous (yet critical) foundations like data integration, compliance, and user training. The healthcare software market’s rapid growth and the industry trends discussed (from value-based care to patient consumerism) make it clear that organizations who build strong digital competencies now will lead in the coming years.
By understanding the core domains – clinical, administrative, and consumer-facing applications – and staying attuned to trends driving demand, decision-makers can prioritize the right projects. Embracing key enabling technologies, whether deploying an ambient intelligent scribe in clinic or migrating systems to the cloud, will require thoughtful change management but offers substantial rewards in efficiency and patient satisfaction. Equally, recognizing the challenges (privacy, legacy integration, user adoption, etc.) allows leaders to mitigate risks through careful planning and adherence to best practices.
Ultimately, successful custom software initiatives in healthcare share a common theme: they keep people at the center. They use technology not for its own sake, but to support clinicians in delivering better care and to empower patients in managing their health. As you embark on or continue your organization’s digital journey, let this broad perspective guide you. By treating AI as one part of a broad innovation ecosystem and maintaining a clear focus on strategic outcomes and user needs, you can ensure your custom healthcare software projects become resounding successes – improving care, reducing costs, and advancing your mission in the digitally enabled healthcare of the future.
At Pragmatic Coders, we understand the complexities of healthcare technology. With years of experience providing custom healthcare software development services we have helped healthcare organizations navigate digital transformation, streamline operations, and enhance patient care. Our team of experts has successfully built and deployed solutions ranging from patient portals to AI-powered ethnic-aware patient care platforms.
We don’t just write code—we solve real-world healthcare challenges. Whether you need a tailored interoperability solution, a cloud-native AI application, or a workflow automation platform, our end-to-end development process ensures security, compliance, and seamless integration with your existing systems.
If you’re a healthcare executive, digital health innovator, or IT leader looking for cutting-edge custom healthcare software development solutions, we’re here to help.
📩 Contact us today to discuss your project and explore how Pragmatic Coders can turn your vision into reality.
We’ve got answers on anything connected with software development.
Feel free to reach out using the form below, and we’ll get back to you as soon as possible.
You can also schedule an online meeting with Wojciech, our Senior Business Consultant.

founders who contacted us wanted
to work with our team.
